"In-depth knowledge of a condition provides you with the best path to overcome it." — Clare Waismann
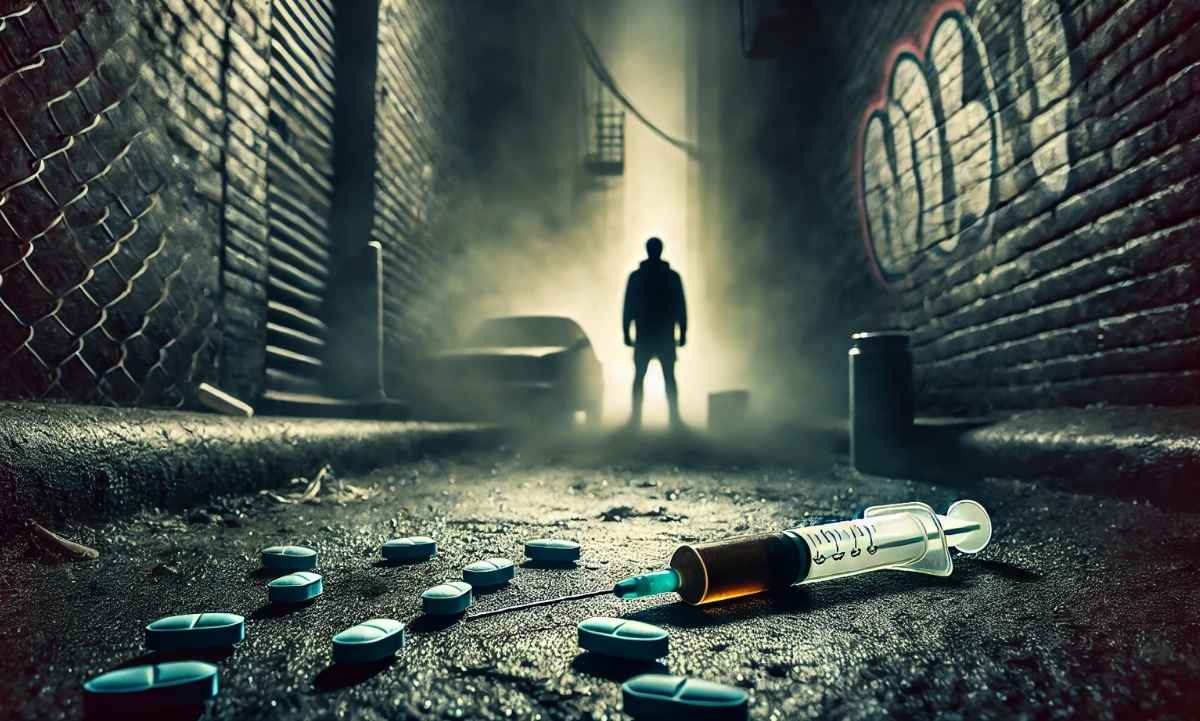
When someone struggles with drug addiction, especially with opioids, it’s all too easy to feel alone. It’s common to feel ashamed, scared and confused. But the truth is, you don’t have to feel isolated in this world. Opioid Use Disorder, is a treatable and common condition, and you have a world of information and support at your fingertips. In this blog, we have compiled a list of relevant subjects to help you become more informed, dispell false myths, and provide you with additional treatment resources.