Naloxone is on the front line as a medicine to combat opioid abuse. With millions of people in the United States suffering from prescription opioid painkiller or heroin abuse, rates of overdose deaths are rising. Naloxone hydrochloride has several potential clinical uses for counteracting the effects of opioids. For example, a naloxone hydrochloride injection rapidly reverses the effects of opioid overdose in a crisis, while naloxone can also be used effectively to treat opioid dependence.
How Does Naloxone Work?
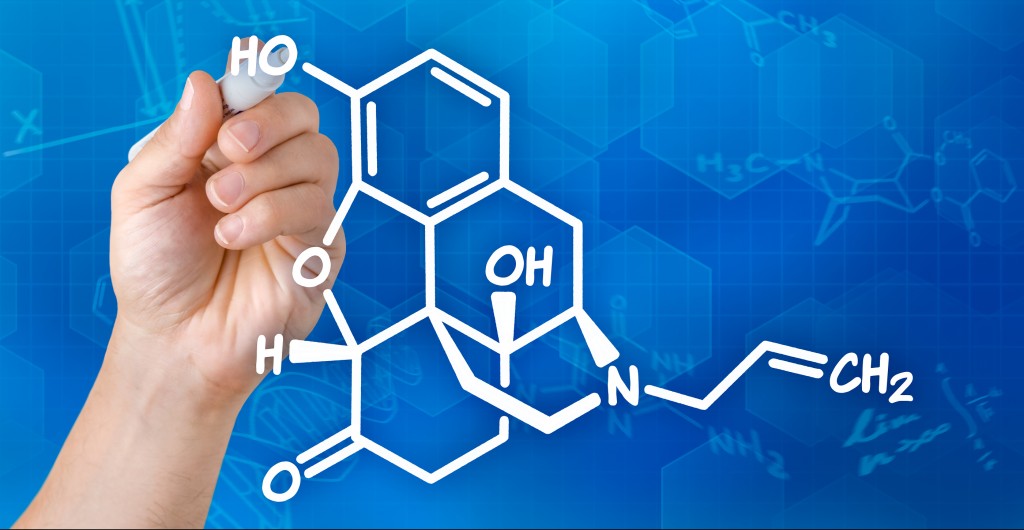
Naloxone hydrochloride commonly goes by the name naloxone, not to mention the trade names, Evzio and Narcan. It is an opioid antagonist, meaning that it opposes the action of opioid molecules in the brain. Furthermore, naloxone is a synthetic compound similar to the drug oxymorphone.
Opioids bind to several types of receptors in the brain. Once there, they have a depressant effect on the central nervous system (CNS) that can be sedating or possibly deadly. However, naloxone hydrochloride has a higher affinity for opioid binding sites than heroin or prescription painkillers. Thus, it knocks these molecules off their receptor sites, reversing the effects of the opioids.
Importantly, naloxone does not have any pharmacological effects of its own. Most importantly, in the absence of opioids, it does not stimulate opioid receptors or has other pharmacological activities that would make it pleasurable to use. This makes it ideal for the treatment of opioid dependence, as it would be undesirable to treat people addicted to opioids with a compound that has a high potential for abuse.
For over 25 years, people from all over the world have chosen Waismann Method as their opioid detox provider.
We know the challenges you face and the importance of creating a unique and personal experience for you right from the start.Call for Detox Options 1-800-423-2482
When created in the laboratory, naloxone hydrochloride appears as an off-white powdery substance. It is available as an intravenous, intramuscular, or subcutaneous injection. Alternatively, individuals can administer it as a nasal spray. In particular, the nasal spray is popular as an accessible, easy-to-administer option for emergency responders or family members of individuals at risk for overdose.
Naloxone Uses
Naloxone for Opioid Overdose
Opioids have a sedative effect, meaning that they slow respiration and CNS activity. This makes it challenging to recognize the signs of an opioid overdose. Common signs include:
- Pale, clammy face
- The person is awake but unable to talk
- Limp body
- The skin turns bluish purple; this may appear as grayish or ashen skin among those with darker skin tones.
- Fingernails or lips turn purple or blue
- Shallow, erratic, or stopped breathing
- Slow or erratic heartbeat. In serious situations, the pulse may stop.
- A “death rattle” sounds, such as choking or gurgling
- Vomiting
- Loss of consciousness
- Lack of response to any outside stimulus (e.g., unable to respond to loud noise or bright light)
When emergency medical responders suspect an opioid overdose, they may administer a naloxone hydrochloride injection. Next, the naloxone quickly travels through the blood, crosses the blood-brain barrier, and replaces opioid molecules at their receptors. Moreover, this effectively reverses the overdose, causing a person’s breathing and heart rate to increase.
Naloxone and Preventing Opioid Abuse
Opioid abuse is a pattern of problematic drug-seeking behavior. Naloxone is sometimes used to prevent opioid abuse. For example, buprenorphine is commonly combined with naloxone to create drug Suboxone. Suboxone is prescribed to individuals suffering from opioid abuse to reduce withdrawal symptoms while a person undergoes treatment for opioid abuse. Because buprenorphine has abuse potential, naloxone is included in Suboxone for the purpose of preventing Suboxone abuse.
Naloxone and Rapid Detox
Opioid dependence is a condition in which the body physically depends on opioids for normal functioning. For instance, we characterize dependence by tolerance or withdrawal. Tolerance refers to needing higher doses of the drug to achieve the same effects. Whereas, withdrawal refers to symptoms that arise when it has been a while since a person has gotten the drug. In other words, these signs indicate that a person’s body has physiologically changed to depend on opioids for everyday functioning.
One of the challenges in treating opioid dependence is that withdrawal symptoms are unpleasant and may even be dangerous. For instance, opioid withdrawal involves gastrointestinal distress, runny nose, anxiety, agitation, and muscle aches. However, rapid detox protocols are designed to speed the withdrawal process, making it easier for a person to overcome opioid dependence. Rapid detox involves the administration of naloxone in a safe, medically supervised environment. Naloxone sweeps opioid molecules from their receptors in the brain, causing physical detoxification within a period of hours. In conclusion, this allows patients to overcome withdrawal and focus on recovery from addiction.
Counteracting the Nation’s Opioid Epidemic
When used appropriately, naloxone can be an effective part of counteracting the nation’s opioid epidemic. Expanding access to effective treatments such as rapid detox can help affected individuals get the help they need. To the question, can naloxone save your life? the answer may very well be yes.
Sources
Expanding Naloxone use could reduce drug overdose deaths and save lives, Center for Disease Control. Retrieved on March 29, 2016.
Naloxone. Drugs.com. Retrieved on March 29,2016.
Recognizing Opioid Overdose. Harm Reduction Coalition. Retrieved on March 29,2016.