As Seen in The Media

Friday, April 26th, 2019
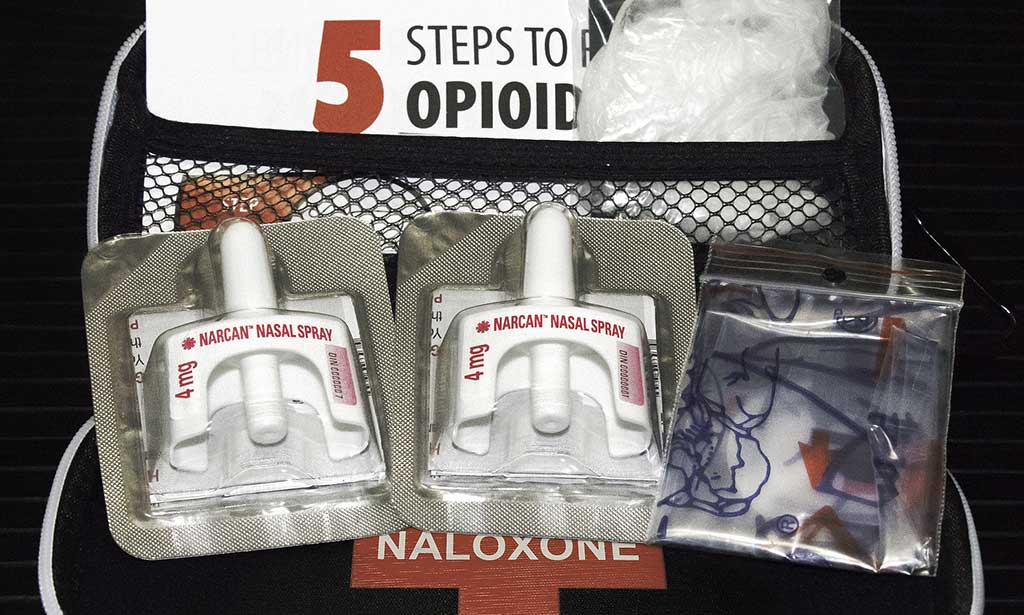
National Drug Take-Back Day: Your Medicine Cabinet Is a Source for Opioid Abuse
Stolen, misused and lost prescription drugs fall into the wrong hands or end up as environmental hazards. That’s why the Drug Enforcement Administration (DEA) launched National Drug Take-Back Day....
Read More